Evidence-based medicine is a method of systematically testing interventions to empirically validate which are the most effective. These practices have been the standard in the medical field for decades, but have only somewhat recently become a focus for behavioral healthcare providers.
Behavioral health contains a number of complexities not found in the world of physical health, making adoption much more difficult. Within standard medicine, simple scans can determine if the patient’s underlying condition has been cured or at least if there has been improvement. In behavioral health, no such scans are available. Instead, practitioners and researchers are reliant on subjective patient reports.
Other complexities also exist, such as a lack of standardization in care delivery, large numbers of variables that affect patients’ mental health outside of the provider’s or researcher’s control, and long recovery timelines, to name a few.
Still, much has been learned about what works for patients. We know most patients’ mental health improves with treatment and we know that individuals can fully recover from issues ranging from substance use disorder to schizophrenia.
In this article, we’ll outline what the research to date tells us has a positive impact on patient outcomes, looking at both programmatic and individual clinician-determined factors.

Building an Evidence-Based Program
Many providers may feel they already have an evidence-based program in place, but Brandon George, the Director of Consulting with Ascension Recovery Services and previous Executive Director for the Indiana Addiction Issues Coalition, pointed out that providers in Indiana still had work to do:
“I think broadly, evidence-based practices provide some standards and guardrails for providers getting into the [addiction treatment] space. If you look at the industry as a whole, it was run by a bunch of folks in recovery in the 70s, 80s, and early 90s, until the state stepped in and created licensure around this as opposed to just the certifications that they had. It provided standards that were really needed at the time. There are also some really good emerging practices that are not necessarily considered that last layer of evidence-based. I think there are three terms for where things are at in the process, such as evidence-informed. It is important to leave space for those doing innovative work. A lot of facilities are checking the box and saying they do evidence-based practices, but their application is not always well implemented or understood.”
There are numerous programmatic elements that increase the likelihood of patients achieving lasting recovery. Length of treatment, levels of care, aftercare programming, combining pharmacological interventions, and internal training processes all have effects on patient outcomes. We’ll take a look at each along with corresponding research.
Length of Stay
When it comes to length of stay, different patients will require different time frames based on the nature of their addiction, and factors such as undiagnosed mental health conditions. As professionals, we understand that when patients stay connected to care, they have a better chance of finding success in recovery.
Based on The National Institute on Drug Abuse’s “Principles of Drug Addiction Treatment: A Research-based Guide (3rd Edition),” the following timelines are important:
- 3 months in formal treatment (across levels of care)
- 12 months connected to treatment or treatment-related support
- Often more than one episode of formal treatment with the average patient needing between 2 and 5 episodes of care, not necessarily at high levels
- Full continuum of care – withdrawal management (detox), inpatient, outpatient, and aftercare
A key factor here is the length of time connected to care. No one level is generally sufficient. Instead, the severity of presentation determines at what level of care a patient enters treatment. Additionally, all patients benefit from the lengths of time connected to care referenced above. This is particularly important for some patients who regard detox as a singular treatment. Most patients feel “better” after detoxing and have a false sense of “being cured.” Behavior change is hard, as anyone who has ever made a New Year’s resolution to start going to the gym or dieting knows. Those managing addiction need extended care and support in order to achieve their recovery goals.
Studies indicate that return to use is common within the first 90 days of leaving treatment and within the first 12 months. This is why full continuums that include general outpatient, beyond the usual PHP and IOP levels of care, are important. Staying within a single system of care, rather than transferring providers, also comes with many benefits such as ease of patient record transfer, communication linkages between levels of care, continuity in programming, and patient familiarity with the program.
The referenced studies also further emphasize the importance of patients staying connected to care even after completing formal treatment. Alumni programs, traditional support groups, and peery recovery coaches are all important options for patients to continue their recovery surrounded by their peers.
Mr. George also shares his opinion on the continuum of care and how important addressing non-medical needs is for those in recovery:
“We are built around this 30-day residential model, but the idea that someone spent 20 years dragging their life down and then we give them 30 days and tell them they are good to go doesn’t work. Addiction is chronic, and it will take an extended period to help somebody get all of their determinant markers up and into place. Once someone hits a year of recovery, the odds of staying healthy are much better. Three years is another solid marker but at five years, that person has the same percentage chance of returning to use as the average person does for developing SUD. So that should be the marker, how do we get people to five years? You don’t need detox at four years, but you might need job training, nutrition, exercise, or other areas of support in your life. What do people need in recovery in years 2-5? This is where tracking outcomes is needed, because how are you supposed to know what someone at 18 months in recovery needs?”
This is why RCA commits to a full continuum of care including standard outpatient and extensive alumni services in addition to assisting patients to find recovery support groups near their home.
Medication for Addiction Treatment (MAT)
Over the past decade, a growing body of evidence shows that MAT for opioid use disorder (OUD), sometimes referred to as medication for opioid use disorder or MOUD, is highly effective at reducing overdose deaths and helping patients find long-term recovery. After three months, of those who adhered fully to a MAT program, only 3.6% experienced a nonfatal overdose. Compared to those who did not adhere, 13.2% experienced a nonfatal overdose. These numbers are the key to understanding how effective MAT can be. Those who do not adhere to the MAT program are 3.5 times more likely to experience an overdose. This creates a rise in the cost of healthcare for patients as well.
The data surrounding MAT further shows that it is an effective, evidence-based treatment in addressing OUD. Patients who attend detox only show little-to-no improvement in terms of long-term recovery. The goals of MAT are not just to improve patient outcomes as far as treatment, but to also improve their overall health and well-being. A collection of literature known as The Assessing the Evidence Base (AEB) supports these statistics in studies from 1999-2012. Some areas where improvements were noticed include:
- Criminality
- Mortality
- Reduced risks of drug-related HIV/Hepatitis C
In Indiana, Medicaid began covering OUD services and treatments in 2018. At that time, 52,994 Medicaid enrollees were diagnosed with OUD or had an opioid-related event. However, only 5.41% received a form of treatment, including MAT. Between the stigmas surrounding MAT and the lack of resources (such as childcare, transportation, etc.), not enough Hoosiers are utilizing MAT to treat OUD. Patients at Recovery Centers of America receive MAT while enrolled in treatment, while clinics such as CleanSlate are serving Indiana communities with MAT program options.
Dr. James Meacham, the Regional Medical Director for CleanSlate in Indiana, has been helping patients with OUD for over three decades. He had the following to say about their program and MAT for OUD:
“Medication for Opioid Use Disorder (MOUD) is clearly effective and saves lives. We are seeing an increase in access to care as well as lower thresholds of cost. The stigmas behind MOUD are also decreasing. In our environment, we strongly encourage our patients to enroll in behavioral and mental health treatment as well as support groups. Those relying on MOUD alone are less likely to maintain and sustain recovery.”
Cravings and withdrawal symptoms are particularly challenging for patients struggling with OUD. Using medication to counteract these effects has proven extremely efficacious in helping patients adhere to recovery programming.
Ongoing Clinical Training and Feedback
For a provider to consider themselves as utilizing evidence-based therapy and techniques, ongoing feedback and clinical training are critical. Without continuous education and training, therapists may:
- Have plateaus in proficiency
- Obtain slightly worse patient outcomes over time
- Become overconfident, which also leads to worse patient outcomes
To see improvement in patient outcomes, ongoing training is a necessity. Studies have shown that therapists who are only self-assessing show slight declines in patient outcomes over time. Therapists are also less likely to feel supported in their career goals when regular auditing, feedback, and coaching are lacking. By implementing regular session audits from a supervisor followed by feedback and coaching, programs can support therapists in their own personal growth goals while, at the same time, maintaining and improving patient clinical outcomes.
The key to building and implementing these skills is through feedback. After a supervisor performs a session audit, discussing with the therapist the areas that need improvement will allow them to engage in deliberate practice. The goal is to build the therapeutic alliance with the patient, but without hearing feedback, the therapist has no way to make adjustments, as studies have shown self-reflection alone is unlikely to produce improved outcomes among therapists. Supervisors are able to address areas of concern and help give guidance for the therapist to improve.
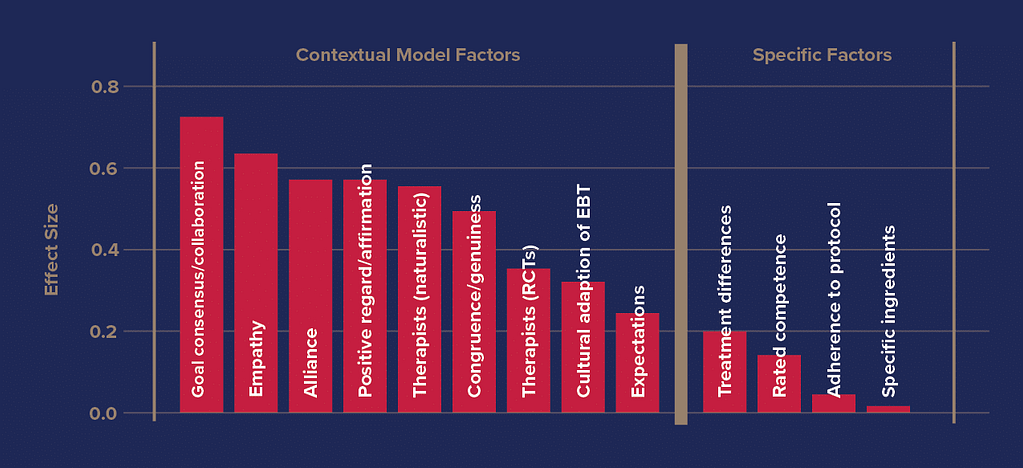
There are seven main skills areas identified in the research through which therapists can improve to obtain better outcomes with their patients. These are: alliance, empathy, goal consensus/collaboration, positive affirmation, genuineness, expectation in therapy, and cultural adaptation of evidence-based treatment. By having clear definitions of what skills fall into these categories, supervisors can pinpoint specific areas that need improvement as opposed to broad-spectrum answers such as “communication needs to improve.” In this example, communication with patients could mean empathetically, collaboratively, or genuinely. Strong supervision provides actionable guidance the supervisee can use to improve their practice.
At Recovery Centers of America, we provide constant and ongoing training for our staff as well as session audits and feedback. The goal is to help professionals constantly grow, improving the skills that matter most.
Improvement must also be measurable. Evidence-based programs use actual outcomes data in order to determine what is and isn’t working for patients within the program.
Outcomes Tracking
Outcomes tracking gives a clear insight into what practices are proving successful and the areas that need improvement. However, a study from the International Journal of Mental Health Systems indicated that when first presented with tracking software – in this case, the tracking software was Norse Feedback, commonly used in Norway – therapists were reluctant to accept a new practice. After implementing the software, the therapists reported that the most frequently used areas of the program were the alliance and patient-reported therapeutic needs sections. These were the areas needed most during sessions to understand what patients wanted from their treatment. The study took place over 18 months, and found that the Norse Feedback software assisted the therapist in addressing clinical needs for patients.
At RCA, Owl Health is used and is an objective third-party patient outcomes platform. Darius Brannon, Clinical Director at RCA Indianapolis explains “Owl is all about measurable outcomes. The therapist uses the Owl screeners (GAD-7, PHQ-9, and BAM). Each of these psychometric screeners helps the therapist individualize treatment and track the patients’ progress or lack thereof. The Owl system is a very helpful tool.”

Evaluations do not always guarantee patient success, nor can they predict how each individual will respond to each practice. However, when each individual therapist implements changes through feedback, the improvement in their practice will be noticed by patients.
Tailoring Treatment by Matching Patients with the Right Therapist & Program
As previously discussed, collaborative goal setting is an important factor in predicting patient improvement. For example, pairing a therapist who incorporates spirituality into their treatment methods with a patient of a similar mindset is more effective than pairing a spiritual therapist with a patient who identifies as an atheist. Without being able to align on goals and treatment approaches, the patient is unlikely to stay in treatment or follow their therapist’s guidance.
Despite actively seeking care for mental health, more than 60% of patients do not feel they benefit from the care they are receiving. A program in Australia committed to evidence-based care found that matching therapist skills with the patient’s area of need led to significantly improved patient outcomes.
By the same token, matching patient needs to specific programming should have an equally positive effect. This is why RCA has three pathways for patient programming. The first is for those who are in treatment for the first time. The second is for those reentering treatment after returning to use. The third is for those with co-occurring disorders. By pairing patients not only with therapists who fit these individual needs but also surrounding patients with like-minded peers, we have seen stronger patient outcomes through this method.
Tailored programming for veterans, LGBTQ+, members of specific faiths, etc. are likely to work in a similar fashion. Beyond the program level, each therapist is then best able to tailor programming to meet the specific needs of individual patients. Just as we have research on what works programmatically, we also have research on what works in terms of individual interventions by therapists.
The Impact of Individual Therapists
Research indicates that only about 7% of treatment outcomes are related to the impact of individual therapists. While this may seem small, it is the largest in-program effect size, meaning that the quality of interventions provided by therapists is the most important factor in helping individual patients progress. In this section, we’ll examine what actions research indicates individual therapists can take to positively impact patient outcomes.
Outcomes Tracking and Clinical Feedback Loops
By constantly assessing patients using psychometrically validated instruments such as the GAD7, PHQ9, or BAM, therapists can better understand how patients are progressing or catch red flags early in order to provide additional interventions. More importantly, therapists can test whether or not a particular intervention is working for a particular patient. Therapists can quickly course correct when an applied intervention is not obtaining the desired outcome.
In a recent study looking at patients who are at high risk for treatment failure, patient feedback given to therapists proved effective. The rate of patient failure reduced from 25% in the control group to 8.7% in the group providing feedback. The study used an outcome questionnaire which was self-reporting.
Patient feedback can be as simple as filling out surveys after sessions or using data tracking software programs, and gives a deeper insight into what practices are working. When patients first enter therapy, typically they do not know what to expect from treatment. Continuous monitoring through surveys not only allows the therapist to understand how the treatment is going, but gives patients a way to see progression.

Deliberate Practice of the Skills That Matter Most
Collaborative goal setting, building a therapeutic alliance, and empathy are the three most important skills for any therapist to master that have a strong impact on patient outcomes. By focusing on deliberate practice and honing in on areas of improvement, the skills will become second nature and delivery will become more efficient.
In a study performed by Benjamin Bloom, he noted that “experts are always made, not born.” By looking into the elite performers, he saw the consistency and intensity in practice that led them to be at the top of their field. The same can be applied to therapists. By putting in the time and dedication but not rushing through, expertise will continue to develop throughout the process.
Deliberate practice does not just mean reading books in free time. The key to proper implementation of deliberate practice revolves around core principles: analyzing sessions via audio or transcription, feedback from a supervisor on areas of improvement, and repeatedly practicing cognitive and intervention skills at the level of development. Mastering any skill, craft, art, or subject takes time, patience, and repetition, and becoming an expert does not mean practice ends. Therapy is a form of medicine, it is always developing and evolving, meaning practice never stops.
The most effective therapists understand what skills are important in delivering outcomes, monitor their proficiency in using those skills with patients, and compare assessed patient outcomes over time. They lean into what they’re good at, but ensure they’re constantly improving in the areas where they aren’t as strong, testing a practicing technique until patient outcomes improve even further.
Building Patients’ Skills & Recovery Capital
As noted earlier in this article, in-program effect sizes are comparatively small. The largest factors influencing success or failure in recovery occur outside of the four walls of therapy. Life circumstances such as socioeconomic status, family dynamics, physical health, and access to resources, among other factors, all have a strong effect on patient outcomes.
With this in mind, effective therapy is not simply a process of alleviating symptoms in treatment. Patients must be able to succeed in the real world outside of the four walls of therapy by navigating life circumstances that exist as barriers to long-term recovery.
By equipping patients with real-world skills to address conflict, achieve goals, regulate emotions, etc., therapists can empower patients to navigate whatever challenges life throws at them in the real world. Andrew Bordt, the executive director of The Institute for the Advancement of Group Therapy, shares his view on building patient skills within the treatment setting:
“In the neuroscience of recovery, it’s ‘fire it to wire it.’ If you think about something like substance use, those pathways are strongly linked in the brain already. Like walking to a destination in the forest, the first couple of times you’re just crunching over grass and leaves. But if you keep doing it over and over again, a groove is worn into the dirt. And eventually, that groove will become a trench. And so, that’s very easy to fall into and that is why bad habits are so hard to break. But, it is not impossible to form new neurological pathways in terms of thoughts, behaviors, or life skills. In therapy, we’re trying to create and strengthen new neural pathways. But this must go beyond just different ways of thinking. Patients need recovery related skills to enable their success in the real world outside of treatment. If we can get those habits formed really well in treatment, then patients can face whatever life throws at them at the times when they don’t have a supportive therapist by their side.”
Length of stay also has a strong effect on patient skill-building due to the “fire it to wire it” principle of neurobiology. Thought patterns, behavioral changes, and other skills require extensive repetition over time. When patients have the time to practice skills correctly and effectively, they have a better chance of implementing them outside of treatment. Additionally, frequent repetition leads to automaticity. When an individual is faced with a stressful situation or conversation in the real world, they need their brain to default to rapid-response, automated behaviors. In difficult situations, they don’t have time to stop and consciously think through the copying skills they were taught.
As Mr. Bordt continues, “In this way, it’s not just about time in treatment, but how that time is used. A lot of time in treatment needs to be used to actively practice skills so that patients have achieved a certain level of automated proficiency before completing the program. Automated proficiency only comes from repeated practice.”
Conclusion
As we’ve seen, evidence-based programs incorporate both programmatic elements and specific approaches to treatment by individual clinicians. Evidence-based is not just a term – it is a way to put our best foot forward and truly see through data tracking the benefits of therapy, aftercare, and return to use prevention. Recovery Centers of America is at the forefront here in Indiana, working to encourage providers to look into their practices and strive for improvement every step of the way. We fully believe that to be successful in the SUD and mental health fields, we must push ourselves to keep learning and developing strategies for improving patient outcomes.
A successful patient outcome is the reason we do what we do. At Recovery Centers of America, we tailor our programs to ensure each individual is set up to achieve the path of recovery. To learn more about the mission of evidence-based treatment from Recovery Centers of America, call (855) 761-2897.
Source Links
- https://nida.nih.gov/sites/default/files/675-principles-of-drug-addiction-treatment-a-research-based-guide-third-edition.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6602820/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2211734/
- https://www.sciencedirect.com/science/article/pii/S0740547218305488
- https://ps.psychiatryonline.org/doi/full/10.1176/appi.ps.201300235
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9982140/
- https://div12.org/do-psychotherapists-improve-with-time-and-experience/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9606408/?fbclid=IwAR0it6IiOcDiJ32aMlyuAcjmI07QfO0LKP-spEii1O6KAgAUNAzQFyZ4nvI
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4592639/
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2780658
- https://psychology.org.au/for-members/publications/inpsych/2020/aug-sept-issue-4/improving-practice-outcomes
- https://www.sciencedirect.com/science/article/abs/pii/S0022399913002699
- https://www.apa.org/monitor/2023/06/measurement-based-care-patients-treatment
- https://www.psychologytoday.com/us/blog/parenting-from-a-neuroscience-perspective/202303/the-neuroscience-of-effective-practice
- https://hbr.org/2007/07/the-making-of-an-expert
- https://deliberatepracticeinpsychotherapy.com/deliberate-practice/Imel, Z., Wampold, B. (2015) The Great Psychotherapy Debate: The Evidence for What Makes Psychotherapy Work (2nd Edition). New York. Routledge.

